Known as the ‘Sunshine Vitamin’, what roles does Vitamin D have within the human body, how do we produce it and should we supplement with it? We explore Vitamin D in depth and help you to learn more about its role in immunity, health and exercise performance.
Vitamin D was discovered in 1913 when researchers were trying to identify the cause and treatment of rickets, a disease that became known as the ‘The English Disease’ due to its prevalence within England and other British nations. Rickets is a disease which results in soft bones due to a lack of Vitamin D, calcium and phosphates from within the diet, which when available in sufficient quantities, contributes to optimal bone health, strength and development.
It wasn’t until the 1950’s where the role of Vitamin D within the human body started to become more understood. Around this time, Vitamin D was considered as a ‘Co-enzyme’, meaning that it would work alongside other enzymes as a catalyst to start and control chemical reactions. As research advanced, the idea of Vitamin D as a co-enzyme dwindled and Vitamin D was soon considered a ‘pro-hormone’. Simply put, being a pro-hormone means that Vitamin D can start a chemical reaction, rather than control the rate of the reaction, which is the role of an enzyme (DeLuca.F, 2014).
Intriguingly, Vitamin D is known as ‘the vitamin that’s not a vitamin’ (This isn’t as confusing as it may sound). Vitamin D was given its title during a period of time where other dietary vitamins were being discovered and identified, such as Vitamin A, and thus it was incorrectly labelled as a vitamin. This is because vitamins are classified as substances that cannot be produced by the human body and therefore must be sourced from the diet. Yet Vitamin D can be produced by the body, via the conversion of UVB radiation from sunlight within the skin, whilst also being found in very small quantities within certain foods, such as oily fish (Larson-Meyer and Wallis, 2010). Vitamin D is produced after UVB rays from sunlight are absorbed by the skin. Once sent to the liver and kidneys, Vitamin D is converted into Vitamin D3, the active form of the Vitamin D, which provides the physiological benefits that are to be discussed throughout this article.

The interest in Vitamin D on human health has significantly increased over recent years due to the discovery of Vitamin D receptors, which have been located across a vast array of cells within the body. This suggests that Vitamin D could play an essential role in regulating many different cell functions, which from a health and exercise perspective could be highly influential, especially to sports performance. Vitamin D is also widely understood to enhance the innate and adaptive immune systems (you can learn more about how the immune system functions in our Immune System Support Resources). It also contributes to skeletal muscle performance, development of muscular strength and also cardiac function which are all significant areas of interest for athletes and physically active people.
Vitamin D3 Production from Sunlight: According to Owens et al (2014), as the skin is exposed to UVB radiation, the process responsible for converting the UVB radiation into Vitamin D3 starts within the liver. After 8 hours, 80% of the Vitamin D from UVB is converted into the active Vitamin D3 form. 90% of the Vitamin D3 in the human body comes from sunlight, with only a microscopic 10% coming from the foods we eat such as oily fish, eggs and cereals fortified with Vitamin D.
Some foods will contain Vitamin D2, a less active form of Vitamin D. Vitamin D3 has been shown to be 9.5x more potent than Vitamin D2 in raising blood Vitamin D concentrations and therefore only 20 to 30 minutes of sun exposure on the face and arms in summer months is enough to satisfy the daily requirements for Vitamin D.
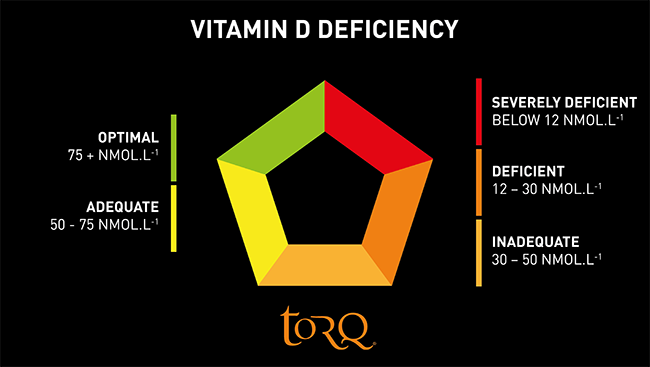
Factors Leading to Vitamin D Deficiency: A recent review article from Lips and colleagues (2019) summarised that up to 60% of Western, Eastern and Southern European populations show blood concentrations of Vitamin D at less than 50nmol.L-1, putting these individuals into inadequate, deficient, and severely deficient categories. Interestingly, up to 80% of Middle Eastern populations also fell into this same level of deficiency, yet these countries typically have extended periods of sunshine, especially throughout the summer months, so how could it be possible that these populations are deficient in Vitamin D?
Firstly, if we consider those large populations living in a geographical location around 40 degrees north of the equator (eg. Europe, North America, Russia), these are locations which typically have less sunlight, especially during winter months of October to March where daylight hours are significantly reduced (even further north in the less populated Scandinavian countries and Canada, daylight hours are fewer still). This reduction in daylight hours caused by seasonal variation is a clear reason for Vitamin D deficiencies in these populations. This then brings us on to the next question of what happens if we have a lovely, sunny day in the winter? According to Chen et al (2007), as much as we would like to think that this is enough to stimulate Vitamin D production, unfortunately the angle of the sun to the earth (scientifically known as the solar zenith angle) is not direct enough for the UVB radiation to reach the earth’s surface and thus be absorbed by human skin. Therefore, even athletes and physically active people who spend lots of time outdoors in winter months are still at risk of becoming deficient in Vitamin D.

A simple yet effective way to determine if the sun is at the correct angle for optimal Vitamin D absorption is to consider your physical shadow size. When standing outdoors on a sunny day, if your shadow is shorter then you, then you will be in optimal conditions for Vitamin D production, however, if your shadow is longer than you, then it is highly likely that the sun is not at a sufficient angle to the earth for the UVB radiation to reach the earth’s surface and thus you will not be able to produce Vitamin D3.
Secondly, there is evidence that populations residing in the Middle East or locations closer to the equator (0 – 40 degrees latitude) show a greater risk to becoming deficient in Vitamin D than those residing in Western, Eastern or Southern Europe (80% – 60% respectively). This could seem highly contradictory based upon the understanding that the Middle East and areas around the equator would be exposed to large amounts of sun light and UVB radiation daily, based on the annual solar zenith angle. However, a key consideration here is the environmental temperature throughout the day and when athletes and general populations alike may choose to complete their outdoor activities. This tends to be at dawn or dusk, when the temperature is much cooler, thus avoiding the extreme heat and powerful daytime UVB radiation from the sun.
Another interesting consideration is the human evolution of a person’s skin pigmentation. People who originate from areas residing between 0 and 40 degrees latitude have evolved to naturally block UVB radiation through developing darker skin pigments. This would mean that to absorb the same amount of UVB, an individual with darker skin would have to spend a greater amount of time in the sun compared to an individual with lighter skin.
And then there’s the issue of spending time in the powerful sun and the effect it may have on our skin health. As we all know, frequent and long periods on sun exposure without UV protection from sun screen can have significant, detrimental effects on our skin health, with the most concerning factor being the potential development of skin cancers. With this in mind, health authorities stress how critical it is to protect your skin from the sun – to remember to ‘cover up’ and wear UVB protection via sun screen creams. Therefore the perfect paradox exists, whereby the wearing of clothing and UV protection creams to prevent damage to the skin from the sun also prevents UVB radiation from being absorbed by the skin and therefore affecting the rates of Vitamin D production.

The recent effects of the Covid-19 pandemic may have also lead to individuals developing a deficiency in Vitamin D due to the government enforced “stay at home” message. This resulted in far fewer people travelling to work who would have once walked or cycled, especially those living in towns or cities. With many workplaces noticing an increase in efficiency from staff members working from home and many homeworkers enjoying the benefits this brings, this new way of work could form ‘the new normal’ and bring with it ongoing Vitamin D deficiency issues. A paradox yet again with Covid – a nutrient essential for immune health is reduced as a result of locking-down at a time when it’s needed most!
Identifying Vitamin D Deficiency: The most accurate method of determining if you are deficient in Vitamin D is to complete a home test which can be purchased from your local pharmacy. To do this you would be required to take a small (teardrop sized) sample of blood from your fingertip and sample this blood using the analyser provided. You would then need to wait around 20 minutes while the analyser quantifies the results. Although a home test could cost between £20 – £50, this is the most accurate way to determine your Vitamin D status and develop a clear understanding of whether you should be supplementing with Vitamin D and of course, how much Vitamin D you will need to correct your deficiency.
Admittedly a home test isn’t essential, and therefore a second method of determining the risk of deficiency is to complete a tick sheet questionnaire identifying specific risk factors such as time spent indoors, the location in which you live and the degree of protection offered by your skin pigmentation. Of course, the more risk factors you tick, the more likely you are to be deficient in Vitamin D. An example of this questionnaire can be seen below.
| Vitamin D Deficiency Risk Factor | Yes | No | |
|---|---|---|---|
| Do you spend less than 2 hours outdoors a day? | Yes | ||
| Do you actively avoid sunlight during the day? | Yes | ||
| Do you always wear sun block when in the sun? | Yes | ||
| Do you live at a latitude more than 40 degrees? | Yes | ||
| Do you have a dark skin pigment? | No | ||
| Is there an absence of oily fish and eggs within your weekly diet? | Yes | ||
| Do you cover your skin when in the sun with clothing? | No | ||
| Do feel you have a weak immune system? | No |
If you answered YES to:
7– 8 of the questions, you could be at a risk of a “Severe” Vitamin D Deficiency.
4 – 6 of the questions, you could be at risk of being “Deficient” in Vitamin D.
2 – 3 of the questions, you could be on the borderline of adequate and inadequate Vitamin D concentrations.
Less than 2 of the questions, you are unlikely to be deficient.
Lastly, there is a very strong argument to suggest that both of the above methods are completely unnecessary and that you should assume that your Vitamin D levels are low and take a Vitamin D3 supplement anyway. The argument for this approach will become clear as you read on, but in a nutshell, if you live in the UK, you’re going to be deficient in Vitamin D in the winter anyway and in the summer, it’s good solid advice to wear sun protection, so if you follow this, you will be limiting your in-built Vitamin D production then too. The cost of a single test could be as high as 2 years of supplementation too, so why not just take a supplement?
Correcting a Vitamin D Deficiency: Once we have isolated our Vitamin D deficiency, risk of Vitamin D deficiency, or simply assumed that we are deficient, it is important that we know how to increase the concentration of Vitamin D within our blood back to adequate or optimal concentrations. These concentrations out of interest are in the region of 50 – 75nmol.L-1 and to raise Vitamin D levels in a controlled manner, you will need to use a supplement/tablet – specifically Vitamin D3. When supplementing with Vitamin D3 it is critically important that you are familiar with your ‘units required’ to ensure that you are achieving the right amount of Vitamin D from your supplement. These units are measured in either IU’s (International Units) and ug’s (Micrograms). Confusing these two units will give you a very different dose of Vitamin D which could lead to a significant under or over-dose.
For reference, 100IU = 2.5ug, and therefore if you were to confuse IU with ug and supplement on 4000ug thinking it was IU, your daily ingestion of Vitamin D would be 160,000IU – however, this would equate to around a whole bottle of Vitamin D supplements in one dose, so we would hope that this would ring alarm bells that your conversions may be wrong!
Over-dosing with Vitamin D is certainly not dangerous when compared to other supplements such as caffeine and most importantly, over-dosing with Vitamin D to toxic levels would be very difficult to achieve. Work from Owens et al (2014) highlighted that dosing strategies less than 10,000IU per day were rarely associated with toxicity, and it’s only until values of supplementation reach 50,000IU per day for several weeks that negative associations of Vitamin D toxicity start to occur. Although research associates toxicity at 50,000IU per day, the Institute of Medicine and European Food Safety Authority have capped the tolerable upper limits of Vitamin D at 4000IU per day, to prevent the very rare cases of high sensitivity toxicity.
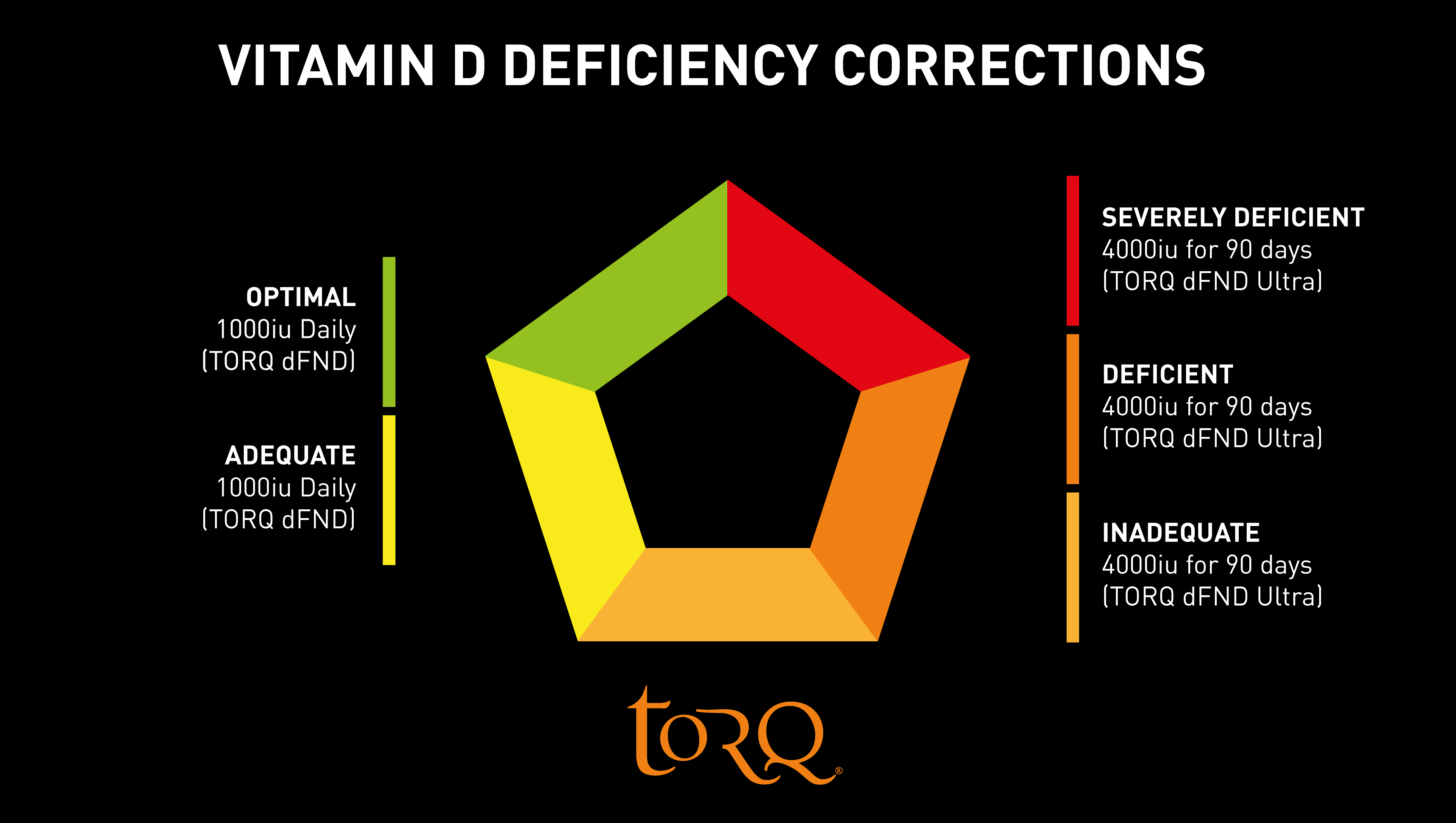
Research from Close et al (2013) who explored dosing strategies to correct Vitamin D deficiencies highlighted that individuals who were severely deficient in Vitamin D showed a much quicker response to Vitamin D correction strategies than those who were only moderately deficient. Additional findings from this paper highlighted that in order to achieve optimal concentrations of blood Vitamin D at values of 75nmol.L-1, a dosing strategy of 2000 – 5000IU per day for 8 weeks would be an effective approach to increase Vitamin D concentration. It’s on the basis of this research that we developed our TORQ dFND products and we highlight in the infographic below how the product range can be utilised to recover a Vitamin D deficiency. Each TORQ dFND ULTRA tablet contains 4000IU of Vitamin D to be taken over 90 days to make absolutely sure that blood concentrations reach the 50 – 75nmol-1 optimal level. Once this is achieved, a daily maintenance dose of 1000IU of Vitamin D from our regular TORQ dFND product ensures that concentrations are maintained. Incidentally, 1000IU is still 500% of the daily NRV (Nutritional Reference Value – formerly known as RDA or Recommended Daily Amount).
TORQ dFND products also contain over 15mg of Zinc, an element also associated with the normal functioning of the immune system and other physiological benefits. To learn more about Zinc, click HERE.
Vitamin D & Immunity: Research from Owens et al (2018) highlights that Vitamin D receptors are found in high quantities in cells responsible for the immune system such as monocytes, macrophages and neutrophils, which suggest that Vitamin D3 plays a pivotal role in the regulation of cells involved in the combat against infection. Not only are these receptors found in high quantities, but research from Liu and colleges (2006) highlighted that Vitamin D also stimulates the production of the cells responsible for the optimal functioning of the innate immune system (the system used for immediate attack against cold, flu and other viruses).
Halliday et al (2011) explored the concept of a Vitamin D threshold on development of the common cold and flu. Athletes who had a circulating Vitamin D concentration of 95m.mol/L-1 or above had significantly less illness episodes than those with Vitamin D values under this threshold. Further research from He et al (2011) also established that endurance athletes with low Vitamin D availability, who encountered symptoms of upper respiratory tract infections, had more symptom days with a greater severity than those with high quantities of circulating Vitamin D.
Further work from He and colleagues, this time from a large participant study published in 2013, highlighted that athletes who were deficient in Vitamin D (Less than 30nmol.L-1) had significantly more episodes of upper respiratory tract infections than those who presented optimal saturations of Vitamin D above 75nmol.L-1, during the winter training months.
Taken together, it’s reasonable to conclude that if you ensure optimal concentrations of Vitamin D within your body, not only do you have a greater ability to recover from illness, but also possess a greater ability to defend yourself against infection. This is why our TORQ dFND product has been so appropriately named.
Research from Gleason (2016) highlighted a very interesting finding supporting the effects of Vitamin D supplementation on Salivary IgA production. If you read our article on Echinacea you can learn more about salivary IgA, however in short, it’s a sticky mucosal layer found in the mouth, larynx and pharynx (throat areas) which acts as a physical barrier against pathogens entering our circulatory system, which can potentially lead to illness. Gleason found that when Vitamin D was consumed at a value of 4000IU per day, Salivary IgA production significantly increased, reducing the risk of illness. Once the Salivary IgA had increased after 3 – 4 weeks of supplementation, participants then moved into a maintenance phase at a dose of 1000IU per day. The suggested dFND protocol involving using dFND ULTRA at 4000IU per day for 90 days followed by regular dFND and 1000IU per day is in line with this research.
Although the primary focus of our TORQ dFND product is on immunity for all, furthering athlete health and performance are key to TORQ’s overall philosophy. From the athletic development perspective, physically active people who experience less interruptions caused by illness can therefore maintain a higher overall training load and consistency, leading to positive training outcomes, such as improved strength and/or endurance. It should also be noted that the benefits of supplementation with Vitamin D3 extends beyond immunity for athletes and physically active people and we will now move on to discuss these.

Vitamin D & Muscular Performance: One of the single biggest factors effecting the ability to perform physically is the efficiency of our muscle during exercise. As discussed in our Cramp Paradox article, calcium plays a vital role in muscular contraction. For a voluntary muscle contraction to occur, a message must be sent from the brain via the central nervous system to the muscle. Once the message has arrived at the desired muscle, the electronic signal stimulates a number of biochemical reactions within the muscle cell, which releases calcium into the muscle fibre and allows the contraction to commence. After considering this very simplified understanding of the mechanisms of a muscle contraction, it is easy to see that calcium regulation plays a fundamental role in the muscle contraction process, and therefore if calcium secretion is compromised, then muscular performance will also be impaired. Vitamin D plays a vital role in the regulation of calcium absorption, so the two are inextricably linked.
Findings from Close et al (2013) found that muscular strength and power tests such as a 10-metre sprint time (running) and a vertical jump height test were improved with supplementation of Vitamin D at dose of 5000IU per day within young athletes. We must consider however that the athletes who were part of this study were all categorised as severely deficient in Vitamin D showing a concentration of below 12.5nmol.L-1 . Large quantities of research have been analysed and used to formulate a single research paper, otherwise known as a meta-analysis. Findings from this meta-analysis has concluded that muscular performance is only improved with Vitamin D supplementation when the athletes blood Vitamin D concentration is below 25nmol.L-1 (deficient).
Although this may suggest that Vitamin D supplementation has little impact on muscular performance unless you’re deficient, we have concluded throughout this article so far that many of us do find ourselves at risk of Vitamin D deficiency. With this in mind, ensuring that our Vitamin D levels are sufficiently elevated rules out any muscular issues we might have by default. Just as Vitamin D supports the normal functioning of the immune system, it also supports the normal functioning of muscle.

Vitamin D on Cardiovascular Strength: As discussed above, optimal Vitamin D concentrations have been shown to impact muscle health and performance which of course could pose really positive implications for athletes and physically active people. Optimal muscle function is critical for almost every single sport type, but optimal muscle function is also important for the general population, specifically elderly populations, when aiming to maintain a good quality of life through proper mobility.
Interestingly, when we discuss the effects of Vitamin D on muscle, we almost always consider our skeletal muscle such the muscles found in our arms and legs, but we rarely consider how Vitamin D may impact our cardiac muscle, specifically the muscle tissues of the heart. Yet the heart, equal to the brain, is possibly the most important organ keeping us alive, so ensuring we have a properly functioning heart is critical to our survival and physical ability.
Research from Allison and Colleagues (2015) explored the effects of Vitamin D concentration on heart size and function in over 800 athletes. The outcomes of this paper were pretty astonishing, highlighting a negative relationship between athletes who were deficient in Vitamin D and the size of their heart. Simply put, athletes who were severely deficient in Vitamin D presented significantly smaller hearts across a range of measurement sites compared to athletes who were insufficient or sufficient in Vitamin D. Of interest too was that 48.5% of the athletes within this study were recorded as being deficient in Vitamin D.
Maintaining optimal heart health is important, and we should ensure we lead an active lifestyle to support our cardiovascular health. Having a stronger heart will allow us to deliver nutrients more effectively, work at higher exercise intensities, deliver more blood per heartbeat and reduce our blood pressure. All of which are factors that can improve exercise performance and our general health.

Summary: Modern lifestyles along with the location in which we live and seasonal variations can have a significant impact on the risk of becoming deficient in Vitamin D. We have established that 60 – 80% of people globally could be at risk of being deficient and as mentioned above, almost 50% of the athletes in the study were deemed deficient too. With many of us being at risk of Vitamin D deficiency, it’s hard to deny that adopting a Vitamin D correction regime by taking 4000IU of Vitamin D for 90 days followed by an ongoing maintenance dose of 1000IU is likely to be of significant benefit to most people.

If you have any questions about this article or any other subject, please don’t hesitate in contacting us at enquiries@torqfitness.co.uk or phone 0344 332 0852.
References:
DeLuca, H.F., 2014. History of the discovery of vitamin D and its active metabolites. BoneKEy reports, 3.
Larson-Meyer, D.E. and Willis, K.S., 2010. Vitamin D and athletes. Current sports medicine reports, 9(4), pp.220-226.
Holick, M.F., 1995. Environmental factors that influence the cutaneous production of vitamin D. The American journal of clinical nutrition, 61(3), pp.638S-645S.
Owens, D.J., Fraser, W.D. and Close, G.L., 2015. Vitamin D and the athlete: emerging insights. European journal of sport science, 15(1), pp.73-84.
Chen, T.C., Chimeh, F., Lu, Z., Mathieu, J., Person, K.S., Zhang, A., Kohn, N., Martinello, S., Berkowitz, R. and Holick, M.F., 2007. Factors that influence the cutaneous synthesis and dietary sources of vitamin D. Archives of biochemistry and biophysics, 460(2), pp.213-217.
Amrein, K., Scherkl, M., Hoffmann, M., Neuwersch-Sommeregger, S., Köstenberger, M., Berisha, A.T., Martucci, G., Pilz, S. and Malle, O., 2020. Vitamin D deficiency 2.0: an update on the current status worldwide. European journal of clinical nutrition, 74(11), pp.1498-1513.
Lips, P., Cashman, K.D., Lamberg-Allardt, C., Bischoff-Ferrari, H.A., Obermayer-Pietsch, B., Bianchi, M.L., Stepan, J., Fuleihan, G.E.H. and Bouillon, R., 2019. Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: a position statement of the European Calcified Tissue Society. European journal of endocrinology, 180(4), pp.P23-P54.
Close, G.L., Leckey, J., Patterson, M., Bradley, W., Owens, D.J., Fraser, W.D. and Morton, J.P., 2013. The effects of vitamin D3 supplementation on serum total 25 [OH] D concentration and physical performance: a randomised dose–response study. British journal of sports medicine, 47(11), pp.692-696.
He, C.S., Handzlik, M.K., Fraser, W.D., Muhamad, A.S., Preston, H., Richardson, A. and Gleeson, M., 2013. Influence of vitamin D status on respiratory infection incidence and immune function during 4 months of winter training in endurance sport athletes.
Gleeson, M., 2016. Immunological aspects of sport nutrition. Immunology and cell biology, 94(2), pp.117-123.
Leary, P.F., Zamfirova, I., Au, J. and McCracken, W.H., 2017. Effect of latitude on vitamin D levels. J Am Osteopath Assoc, 117(7), pp.433-439.
Allison, R.J., Close, G.L., Farooq, A., Riding, N.R., Salah, O., Hamilton, B. and Wilson, M.G., 2015. Severely vitamin D-deficient athletes present smaller hearts than sufficient athletes. European journal of preventive cardiology, 22(4), pp.535-542.
Vazquez, G., de Boland, A.R. and Boland, R.L., 1998. 1α, 25-Dihydroxy-vitamin-D3-induced store-operated Ca2+ influx in skeletal muscle cells: modulation by phospholipase C, protein kinase C, and tyrosine kinases. Journal of Biological Chemistry, 273(51), pp.33954-33960.